Difference between revisions of "Main Page/SlicerCommunity/2019"
Tag: 2017 source edit |
Tag: 2017 source edit |
||
| Line 1: | Line 1: | ||
{{:Main_Page/SlicerCommunity}} | {{:Main_Page/SlicerCommunity}} | ||
=2019= | =2019= | ||
| − | {|width="100%" | + | ==Texture Analysis of Pretreatment <sup>18F</sup>FDG PET/CT for the Prognostic Prediction of Locally Advanced Salivary Gland Carcinoma Treated with Interstitial Brachytherapy== {| width="100%" |
| | | | ||
'''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31511990 EJNMMI Res. 2019 Sep 11;9(1):89. PMID: 31511990] | '''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31511990 EJNMMI Res. 2019 Sep 11;9(1):89. PMID: 31511990] | ||
| Line 11: | Line 11: | ||
'''Abstract:''' BACKGROUND: The aim of this study was to evaluate the prognostic value of positron emission tomography (PET) parameters and the PET texture features of fluorine 18-fluorodeoxyglucose ([18F]FDG) uptake on pretreatment PET/computed tomography (CT) in patients with locally advanced salivary gland carcinoma treated with interstitial brachytherapy. | '''Abstract:''' BACKGROUND: The aim of this study was to evaluate the prognostic value of positron emission tomography (PET) parameters and the PET texture features of fluorine 18-fluorodeoxyglucose ([18F]FDG) uptake on pretreatment PET/computed tomography (CT) in patients with locally advanced salivary gland carcinoma treated with interstitial brachytherapy. | ||
| − | METHODS: Forty-three patients with locally advanced salivary gland carcinoma of the head and neck were treated with 125I interstitial brachytherapy as the sole modality and underwent | + | METHODS: Forty-three patients with locally advanced salivary gland carcinoma of the head and neck were treated with 125I interstitial brachytherapy as the sole modality and underwent <sup>18F</sup>FDG PET/CT scanning before treatment. Tumor segmentation and texture analysis were performed using the '''[http://slicer.org 3D Slicer]''' software. In total, 54 features were extracted and categorized as first-order statistics, morphology and shape, gray-level co-occurrence matrix, and gray-level run length matrix. Up to November 2018, the follow-up time ranged from 6 to 120 months (median 18 months). Cumulative survival was calculated by the Kaplan-Meier method. Factors between groups were compared by the log-rank test. Multivariate Cox regression analysis with a backward conditional method was used to predict progression-free survival (PFS). |
RESULTS: The 3- and 5-year locoregional control (LC) rates were 55.4% and 37.0%, respectively. The 3- and 5-year PFS rates were 51.2% and 34.1%, respectively. The 3- and 5-year overall survival (OS) rates were 77.0% and 77.0%, respectively. Univariate analysis revealed that minimum intensity, mean intensity, median intensity, root mean square, and long run emphasis (LRE) were significant predictors of PFS, whereas clinicopathological factors, conventional PET parameters, and PET texture features failed to show significance. Multivariate Cox regression analysis showed that minimum intensity and LRE were significant predictors of PFS. | RESULTS: The 3- and 5-year locoregional control (LC) rates were 55.4% and 37.0%, respectively. The 3- and 5-year PFS rates were 51.2% and 34.1%, respectively. The 3- and 5-year overall survival (OS) rates were 77.0% and 77.0%, respectively. Univariate analysis revealed that minimum intensity, mean intensity, median intensity, root mean square, and long run emphasis (LRE) were significant predictors of PFS, whereas clinicopathological factors, conventional PET parameters, and PET texture features failed to show significance. Multivariate Cox regression analysis showed that minimum intensity and LRE were significant predictors of PFS. | ||
| Line 21: | Line 21: | ||
==Levator Bowl Volume during Straining and its Relationship to other Levator Measures== | ==Levator Bowl Volume during Straining and its Relationship to other Levator Measures== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31222569 Int Urogynecol J. 2019 Sep;30(9):1457-63. PMID: 31222569] | '''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31222569 Int Urogynecol J. 2019 Sep;30(9):1457-63. PMID: 31222569] | ||
| Line 39: | Line 39: | ||
'''Funding:''' | '''Funding:''' | ||
| + | |||
*P50 HD044406/HD/NICHD NIH HHS/United States | *P50 HD044406/HD/NICHD NIH HHS/United States | ||
*R01 HD038665/HD/NICHD NIH HHS/United States | *R01 HD038665/HD/NICHD NIH HHS/United States | ||
| Line 45: | Line 46: | ||
==Mixed Reality-Based Preoperative Planning for Training of Percutaneous Transforaminal Endoscopic Discectomy: A Feasibility Study.== | ==Mixed Reality-Based Preoperative Planning for Training of Percutaneous Transforaminal Endoscopic Discectomy: A Feasibility Study.== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31203062 World Neurosurg. 2019 Sep;129:e767-e775. PMID: 31203062] | '''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31203062 World Neurosurg. 2019 Sep;129:e767-e775. PMID: 31203062] | ||
| Line 77: | Line 78: | ||
==Prediction of Immunohistochemistry of Suspected Thyroid Nodules by Use of Machine Learning-Based Radiomics== | ==Prediction of Immunohistochemistry of Suspected Thyroid Nodules by Use of Machine Learning-Based Radiomics== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31461321 AJR Am J Roentgenol. 2019 Aug 28:1-10. PMID: 31461321] | '''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/31461321 AJR Am J Roentgenol. 2019 Aug 28:1-10. PMID: 31461321] | ||
| Line 91: | Line 92: | ||
==Technique Development and Measurement of Cross-Sectional Area of the Pubovisceral Muscle on MRI Scans of Living Women== | ==Technique Development and Measurement of Cross-Sectional Area of the Pubovisceral Muscle on MRI Scans of Living Women== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/29974138 Int Urogynecol J. 2019 Aug;30(8):1305-12. PMID: 29974138] | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/29974138 Int Urogynecol J. 2019 Aug;30(8):1305-12. PMID: 29974138] | ||
| Line 114: | Line 115: | ||
==Multi-objective Parameter Auto-tuning for Tissue Image Segmentation Workflows== | ==Multi-objective Parameter Auto-tuning for Tissue Image Segmentation Workflows== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/30402669 J Digit Imaging. 2019 Jun;32(3):521-33. PMID: 30402669] | '''Publication:''' [https://www.ncbi.nlm.nih.gov/pubmed/30402669 J Digit Imaging. 2019 Jun;32(3):521-33. PMID: 30402669] | ||
| Line 125: | Line 126: | ||
'''Funding:''' | '''Funding:''' | ||
| − | * R01 LM011119/U.S. National Library of Medicine | + | |
| − | * U24 CA180924/National Cancer Institute | + | *R01 LM011119/U.S. National Library of Medicine |
| − | * R01 LM009239/U.S. National Library of Medicine | + | *U24 CA180924/National Cancer Institute |
| − | * K25 CA181503/National Institutes of Health | + | *R01 LM009239/U.S. National Library of Medicine |
| − | * UG3 CA225021/CA/NCI NIH HHS/United States | + | *K25 CA181503/National Institutes of Health |
| + | *UG3 CA225021/CA/NCI NIH HHS/United States | ||
|} | |} | ||
==Ancient Machine Tools for the Construction of the Antikythera Mechanism Parts== | ==Ancient Machine Tools for the Construction of the Antikythera Mechanism Parts== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' Digital Applications in Archaeology and Cultural Heritage. 2019 Jun; 13:e00092. | '''Publication:''' Digital Applications in Archaeology and Cultural Heritage. 2019 Jun; 13:e00092. | ||
| Line 147: | Line 149: | ||
==Real-Time Adaptive Planning Method for Radiotherapy Treatment Delivery for Prostate Cancer Patients, Based on a Library of Plans Accounting for Possible Anatomy Configuration Changes== | ==Real-Time Adaptive Planning Method for Radiotherapy Treatment Delivery for Prostate Cancer Patients, Based on a Library of Plans Accounting for Possible Anatomy Configuration Changes== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30818345 PLoS One. 2019 Feb 28;14(2):e0213002. PMID: 30818345] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6394960/pdf/pone.0213002.pdf PDF] | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30818345 PLoS One. 2019 Feb 28;14(2):e0213002. PMID: 30818345] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6394960/pdf/pone.0213002.pdf PDF] | ||
| Line 170: | Line 172: | ||
==Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning== | ==Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://digitallibrary.amnh.org/handle/2246/6924 American Museum Novitates 2019 Feb; 3920:28] | [http://digitallibrary.amnh.org/bitstream/handle/2246/6924/N3920.pdf PDF] | '''Publication:''' [http://digitallibrary.amnh.org/handle/2246/6924 American Museum Novitates 2019 Feb; 3920:28] | [http://digitallibrary.amnh.org/bitstream/handle/2246/6924/N3920.pdf PDF] | ||
| Line 181: | Line 183: | ||
"Segmentation and volume rendering was done using [http://slicer.org 3D Slicer] v4.9." | "Segmentation and volume rendering was done using [http://slicer.org 3D Slicer] v4.9." | ||
| − | |align="right"|[[image:Herhold-AMN2019-fig1.png|thumb|300px|Volume rendering of Lasioglossum (Dialictus) sp. (Halictinae: Halictini), showing location of | + | | align="right" |[[image:Herhold-AMN2019-fig1.png|thumb|300px|Volume rendering of Lasioglossum (Dialictus) sp. (Halictinae: Halictini), showing location of |
abdominal air sacs, displayed as a yellow solid, and “grooves” where metasomal muscles extend into the air-sac space. The insect’s exoskeleton and internal anatomy is rendered translucent, allowing examination of air-sac morphology. The bilateral asymmetry shown here is not uncommon, and usually has to do with how recently | abdominal air sacs, displayed as a yellow solid, and “grooves” where metasomal muscles extend into the air-sac space. The insect’s exoskeleton and internal anatomy is rendered translucent, allowing examination of air-sac morphology. The bilateral asymmetry shown here is not uncommon, and usually has to do with how recently | ||
the specimen has fed. Distension of the gut can occupy space normally taken up by air sacs.]]] | the specimen has fed. Distension of the gut can occupy space normally taken up by air sacs.]]] | ||
| Line 188: | Line 190: | ||
==3D Reconstruction of MR-Visible Fe<sub>3</sub>O<sub>4</sub>-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings== | ==3D Reconstruction of MR-Visible Fe<sub>3</sub>O<sub>4</sub>-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30387537 Neurourol Urodyn. 2019 Jan;38(1):369-78. PMID: 30387537] | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30387537 Neurourol Urodyn. 2019 Jan;38(1):369-78. PMID: 30387537] | ||
| Line 209: | Line 211: | ||
'''Funding:''' | '''Funding:''' | ||
| − | * P50 HD044406/HD/NICHD NIH HHS/United States | + | |
| − | * R21 HD079908/HD/NICHD NIH HHS/United States | + | *P50 HD044406/HD/NICHD NIH HHS/United States |
| + | *R21 HD079908/HD/NICHD NIH HHS/United States | ||
|} | |} | ||
==A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System== | ==A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30426669 J Appl Clin Med Phys. 2019 Jan;20(1):23-30. PMID: 30426669] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6333150/pdf/ACM2-20-23.pdf PDF] | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30426669 J Appl Clin Med Phys. 2019 Jan;20(1):23-30. PMID: 30426669] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6333150/pdf/ACM2-20-23.pdf PDF] | ||
| Line 228: | Line 231: | ||
==Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery== | ==Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery== | ||
| − | {|width="100%" | + | {| width="100%" |
| | | | ||
'''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30635049 J Otolaryngol Head Neck Surg. 2019 Jan 11;48(1):2. PMID: 30635049] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6329078/pdf/40463_2019_Article_324.pdf PDF] | '''Publication:''' [http://www.ncbi.nlm.nih.gov/pubmed/30635049 J Otolaryngol Head Neck Surg. 2019 Jan 11;48(1):2. PMID: 30635049] | [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6329078/pdf/40463_2019_Article_324.pdf PDF] | ||
| Line 251: | Line 254: | ||
'''Funding:''' | '''Funding:''' | ||
| − | |||
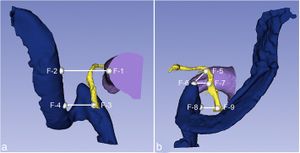
| − | |align="right"|[[image:vanOschJoHNS2019.jpg|thumb|300px| Fiducials and distances calculated from coordinates (BLUE - SS, YELLOW - FN, PURPLE - EAC). a. EAC – SS (F1 – F2); Descending FN – SS (F3 – F4). b. 2nd genu FN – Superior tip JB. (F5 – F6); Descending FN - Superior tip JB (F6 – F7); FN at the SMF - JB (F8 – F9).]]] | + | *381117/Collaborative Health Research Projects |
| + | |||
| + | | align="right" |[[image:vanOschJoHNS2019.jpg|thumb|300px| Fiducials and distances calculated from coordinates (BLUE - SS, YELLOW - FN, PURPLE - EAC). a. EAC – SS (F1 – F2); Descending FN – SS (F3 – F4). b. 2nd genu FN – Superior tip JB. (F5 – F6); Descending FN - Superior tip JB (F6 – F7); FN at the SMF - JB (F8 – F9).]]] | ||
|} | |} | ||
Revision as of 18:25, 18 November 2019
Home < Main Page < SlicerCommunity < 2019Go to 2022 :: 2021 :: 2020 :: 2019 :: 2018 :: 2017 :: 2016 :: 2015 :: 2014-2011 :: 2010-2000
The community that relies on 3D Slicer is large and active: (numbers below updated on December 1st, 2023)
- 1,467,466+ downloads in the last 11 years (269,677 in 2023, 206,541 in 2022)
- over 17.900+ literature search results on Google Scholar
- 2,147+ papers on PubMed citing the Slicer platform paper
- Fedorov A., Beichel R., Kalpathy-Cramer J., Finet J., Fillion-Robin J-C., Pujol S., Bauer C., Jennings D., Fennessy F.M., Sonka M., Buatti J., Aylward S.R., Miller J.V., Pieper S., Kikinis R. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magnetic Resonance Imaging. 2012 Nov;30(9):1323-41. PMID: 22770690. PMCID: PMC3466397.
- 39 events in open source hackathon series continuously running since 2005 with 3260 total participants
- Slicer Forum with +8,138 subscribers has approximately 275 posts every week
The following is a sample of the research performed using 3D Slicer outside of the group that develops it. in 2019
We monitor PubMed and related databases to update these lists, but if you know of other research related to the Slicer community that should be included here please email: marianna (at) bwh.harvard.edu.
Contents
- 1 2019
- 1.1 Levator Bowl Volume during Straining and its Relationship to other Levator Measures
- 1.2 Mixed Reality-Based Preoperative Planning for Training of Percutaneous Transforaminal Endoscopic Discectomy: A Feasibility Study.
- 1.3 Evaluation of Accuracy of a Three-Dimensional Printed Model in Open-Wedge High Tibial Osteotomy
- 1.4 Prediction of Immunohistochemistry of Suspected Thyroid Nodules by Use of Machine Learning-Based Radiomics
- 1.5 Technique Development and Measurement of Cross-Sectional Area of the Pubovisceral Muscle on MRI Scans of Living Women
- 1.6 Multi-objective Parameter Auto-tuning for Tissue Image Segmentation Workflows
- 1.7 Ancient Machine Tools for the Construction of the Antikythera Mechanism Parts
- 1.8 Real-Time Adaptive Planning Method for Radiotherapy Treatment Delivery for Prostate Cancer Patients, Based on a Library of Plans Accounting for Possible Anatomy Configuration Changes
- 1.9 Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning
- 1.10 3D Reconstruction of MR-Visible Fe3O4-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings
- 1.11 A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System
- 1.12 Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery
2019
==Texture Analysis of Pretreatment 18FFDG PET/CT for the Prognostic Prediction of Locally Advanced Salivary Gland Carcinoma Treated with Interstitial Brachytherapy== {| width="100%" | Publication: EJNMMI Res. 2019 Sep 11;9(1):89. PMID: 31511990
Authors: Wu WJ, Li ZY, Dong S, Liu SM, Zheng L, Huang MW, Zhang JG.
Institution: Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Somatology, Beijing, China.
Abstract: BACKGROUND: The aim of this study was to evaluate the prognostic value of positron emission tomography (PET) parameters and the PET texture features of fluorine 18-fluorodeoxyglucose ([18F]FDG) uptake on pretreatment PET/computed tomography (CT) in patients with locally advanced salivary gland carcinoma treated with interstitial brachytherapy.
METHODS: Forty-three patients with locally advanced salivary gland carcinoma of the head and neck were treated with 125I interstitial brachytherapy as the sole modality and underwent 18FFDG PET/CT scanning before treatment. Tumor segmentation and texture analysis were performed using the 3D Slicer software. In total, 54 features were extracted and categorized as first-order statistics, morphology and shape, gray-level co-occurrence matrix, and gray-level run length matrix. Up to November 2018, the follow-up time ranged from 6 to 120 months (median 18 months). Cumulative survival was calculated by the Kaplan-Meier method. Factors between groups were compared by the log-rank test. Multivariate Cox regression analysis with a backward conditional method was used to predict progression-free survival (PFS).
RESULTS: The 3- and 5-year locoregional control (LC) rates were 55.4% and 37.0%, respectively. The 3- and 5-year PFS rates were 51.2% and 34.1%, respectively. The 3- and 5-year overall survival (OS) rates were 77.0% and 77.0%, respectively. Univariate analysis revealed that minimum intensity, mean intensity, median intensity, root mean square, and long run emphasis (LRE) were significant predictors of PFS, whereas clinicopathological factors, conventional PET parameters, and PET texture features failed to show significance. Multivariate Cox regression analysis showed that minimum intensity and LRE were significant predictors of PFS.
CONCLUSIONS: The texture analysis of pretreatment [18F]FDG PET/CT provided more information than conventional PET parameters for predicting patient prognosis of locally advanced salivary gland carcinoma treated with interstitial brachytherapy. The minimum intensity was a risk factor for PFS, and LRE was a favorable factor in prognostic prediction according to the primary results.
|}
Levator Bowl Volume during Straining and its Relationship to other Levator Measures
|
Publication: Int Urogynecol J. 2019 Sep;30(9):1457-63. PMID: 31222569 Authors: Nandikanti L, Sammarco AG, Chen L, Ashton-Miller JA, DeLancey JO. Institution: School of Public Health, University of Michigan, Ann Arbor, MI, USA. Abstract: INTRODUCTION AND HYPOTHESIS: This study was aimed at measuring levator ani bowl volume at rest and while straining, comparing women with and without prolapse (controls), and assessing the ability of measures of the mid-sagittal bowl area, levator hiatus (LH), and urogenital hiatus (UGH) to predict bowl volume. METHODS: Forty MRI scans previously acquired in case-control prolapse studies, including 20 women with prolapse and 20 women without prolapse, of similar age and parity, were selected. 3D models of rest and strain bowl volumes were made using sagittal scans and 3D Slicer. Mid-sagittal bowl area, UGH, and LH were measured using ImageJ. Data were analyzed using two sample t tests, effect sizes, and Pearson's correlation coefficients at the 0.05 significance level. RESULTS: Data were acquired in a total of 40 total women. Levator bowl volume at strain had a correlation coefficient of 0.5 with bowl volume at rest. During straining, prolapse subjects had a 53% larger bowl volume than control subjects (254 ± 86 cm3 vs 166 ± 44 cm3, p < 0.001), but at rest, the difference was 34% (138 ± 40 cm3 vs 103 ± 25 cm3, p = 0.002). Effect sizes for all parameters were large (d > 0.75). The strongest correlation with straining bowl volume was mid-sagittal straining bowl area (r = 0.86), followed by LH strain (r = 0.80), then UGH strain (r = 0.76). CONCLUSIONS: Straining levator bowl volume is substantially different than measures made at rest, with only a quarter of straining values explained by resting measurements. The bowl area at strain is the best 2D measurement estimating bowl volume and explains 74% of straining bowl volume.
|
Mixed Reality-Based Preoperative Planning for Training of Percutaneous Transforaminal Endoscopic Discectomy: A Feasibility Study.
|
Publication: World Neurosurg. 2019 Sep;129:e767-e775. PMID: 31203062 Authors: Yu H, Zhou Z, Lei X, Liu H, Fan G, He S. Institution: Orthopedic Department, Shanghai Tenth People's Hospital, Shanghai, China. Abstract: OBJECTIVE: To explore the effect of preoperative planning using mixed reality (MR) on training of percutaneous transforaminal endoscopic discectomy (PTED). METHODS: Before the training, we invited an experienced chief physician to plan the puncture path of PTED on the X-ray films of the lumbar spine model and the 3D Slicer platform, respectively, and used this as the standard to guide trainees. In the aggregate, 60 young residents were randomly divided into Group A (N = 30) and Group B (N = 30). Group A learned the 2-dimensional standard planning route, whereas Group B learned the standard route planning based on MR through the 3D Slicer platform. Then, trainees were asked to conduct PTED puncture on a lumbar spine model. Questionnaires were distributed to trainees before and after the training. During the training, puncture times, operating time (minutes), and fluoroscopy times were recorded. RESULTS: After the training, it was obvious that more trainees showed their recognition of MR, believing that MR could help preoperative planning and training of PTED. Their high satisfaction with the training indicated the success of our training. Moreover, puncture times, operating time (minutes), and fluoroscopy times of Group B were significantly lower than those of Group A. CONCLUSIONS: MR technology contributes to preoperative planning of PTED and is beneficial in the training of PTED. It significantly reduces puncture times and fluoroscopy times, providing a standardized method for the training of PTED. |
Evaluation of Accuracy of a Three-Dimensional Printed Model in Open-Wedge High Tibial Osteotomy
|
Publication: J Knee Surg. 2019 Sep;32(9):841-6. PMID: 30189435 | PDF Authors: Kim HJ, Park J, Park KH, Park IH, Jang JA, Shin JY, Kyung HS. Institution: Department of Orthopaedic Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, South Korea. Abstract: The purpose of this study was to evaluate the usefulness of a three-dimensional (3D) printed model for open-wedge high tibial osteotomy (HTO). This study retrospectively evaluated 20 patients with medial knee osteoarthritis and varus deformity. Between October 2015 and July 2016, the patients underwent open-wedge HTO using a 3D printed model. The mean age of patients was 55.2 years (range, 51-60 years). The mean preoperative mechanical femorotibial angle (mFTA) was varus 7.8 degrees (range, varus 4.7-11.6 degrees). After measuring the target angle using full-length lower limb weight-bearing radiography, the osteotomy was simulated using 3D images obtained from computed tomography (CT) with the 3D Slicer program. On the basis of the simulated osteotomy section and the target angle, the model was then designed and printed. Open-wedge HTO was then performed by applying the 3D printed model to the opening gap. The accuracy of osteotomy and the change in posterior tibial slope (PTS) angle were evaluated. The weight-bearing line on the tibial plateau was corrected from a preoperative mean of 19.5 ± 9.8% to a postoperative mean of 63.1 ± 6.1% (p < 0.001). The postoperative values were not statistically significantly different from the preoperative target points (p = 0.688). The mFTA was corrected to a postoperative mean of valgus 3.8 ± 1.4 degrees. The PTS angle showed no significant change (p = 0.256). A 3D printed model using CT may be useful for preoperative planning of open-wedge HTO. Satisfactory correction can be obtained without a change in the PTS. |
Prediction of Immunohistochemistry of Suspected Thyroid Nodules by Use of Machine Learning-Based Radiomics
|
Publication: AJR Am J Roentgenol. 2019 Aug 28:1-10. PMID: 31461321 Authors: Gu J, Zhu J, Qiu Q, Wang Y, Bai T, Yin Y. Institution: School of Medicine and Life Sciences, University of Jinan Shandong Academy of Medical Sciences, Jinan, Shandong, China. Abstract: OBJECTIVE. The purpose of this study was to develop and validate a radiomics model for evaluating immunohistochemical characteristics in patients with suspected thyroid nodules. MATERIALS AND METHODS. A total of 103 patients (training cohort-to-validation cohort ratio, ≈ 3:1) with suspected thyroid nodules who had undergone thyroidectomy and immunohistochemical analysis were enrolled. The immunohistochemical markers were cytokeratin 19, galectin 3, thyroperoxidase, and high-molecular-weight cytokeratin. All patients underwent CT before surgery, and a 3D Slicer was used to analyze images of the surgical specimen. Test-retest and Spearman correlation coefficient (ρ) were used to select reproducible and nonredundant features. The Kruskal-Wallis test (p < 0.05) was used for feature selection, and a feature-based model was built by support vector machine methods. The performance of the radiomic models was assessed with respect to accuracy, sensitivity, specificity, corresponding AUC, and independent validation. RESULTS. Eighty-six reproducible and nonredundant features selected from the 828 features were used to build the model. The best performance of the cytokeratin 19 model yielded accuracy of 84.4% in the training cohort and 80.0% in the validation cohort. The thyroperoxidase and galectin 3 predictive models yielded accuracies of 81.4% and 82.5% in the training cohort and 84.2% and 85.0% in the validation cohort. The performance of the high-molecular-weight cytokeratin predictive model was not good (accuracy, 65.7%) and could not be validated. CONCLUSION. A radiomics model with excellent performance was developed for individualized noninvasive prediction of the presence of cytokeratin 19, galectin 3, and thyroperoxidase based on CT images. This model may be used to identify benign and malignant thyroid nodules. |
Technique Development and Measurement of Cross-Sectional Area of the Pubovisceral Muscle on MRI Scans of Living Women
|
Publication: Int Urogynecol J. 2019 Aug;30(8):1305-12. PMID: 29974138 Authors: Masteling M, Ashton-Miller JA, DeLancey JOL. Institution: Department of Mechanical Engineering, University of Michigan, Ann Arbor, MI, USA. Abstract: INTRODUCTION AND HYPOTHESIS: Measurements of the anatomic cross-sectional area (CSA) of the pubovisceral muscle (PVM) in women are confounded by the difficulty of separating the muscle from the adjacent puborectal (PRM) and iliococcygeal (ICM) muscles when visualized in a plane orthogonal to the fiber direction. We tested the hypothesis that it might be possible to measure the PVM CSA within a defined region of interest based on magnetic resonance images (MRI). METHODS: MRI scans of 11 women with unilateral PVM tears and seven primiparous women with intact muscles following elective C-section were used to identify the PVM injury zone defined by the mean location of its boundaries with the adjacent intact PRM and ICM from existing anatomic reference points using 3D Slicer and ImageJ software. Then, from the 15 or more 2-mm transverse slices available, the slice with the maximum anatomic CSA of the left and right PVM was found in 24 primiparous women with bilaterally intact muscles who had delivered via C-section. RESULTS: Mean [± standard deviation (SD)] of the maximum left or right PVM cross-section areas for the 24 women, measured by two different raters, was 1.25 ± 0.29 cm2 (range 0.75-1.86). The 5th, 50th, and 95th percentile values were 0.77, 1.23, and 1.80 cm2, respectively. Inter- and intrarater measurement repeatability intraclass correlation coefficients exceeded 0.89 and 0.90, respectively. CONCLUSIONS: It is possible to use MRI to identify the volume of interest with the maximum anatomic cross section of the PVM belly while minimizing the inadvertent inclusion of adjacent PRM or ICM in that measurement. |
Multi-objective Parameter Auto-tuning for Tissue Image Segmentation Workflows
|
Publication: J Digit Imaging. 2019 Jun;32(3):521-33. PMID: 30402669 Authors: Taveira LFR, Kurc T, Melo ACMA, Kong J, Bremer E, Saltz JH, Teodoro G. Institution: Department of Computer Science, University of Brasília, Brasília, Brazil. Abstract: We propose a software platform that integrates methods and tools for multi-objective parameter auto-tuning in tissue image segmentation workflows. The goal of our work is to provide an approach for improving the accuracy of nucleus/cell segmentation pipelines by tuning their input parameters. The shape, size, and texture features of nuclei in tissue are important biomarkers for disease prognosis, and accurate computation of these features depends on accurate delineation of boundaries of nuclei. Input parameters in many nucleus segmentation workflows affect segmentation accuracy and have to be tuned for optimal performance. This is a time-consuming and computationally expensive process; automating this step facilitates more robust image segmentation workflows and enables more efficient application of image analysis in large image datasets. Our software platform adjusts the parameters of a nuclear segmentation algorithm to maximize the quality of image segmentation results while minimizing the execution time. It implements several optimization methods to search the parameter space efficiently. In addition, the methodology is developed to execute on high-performance computing systems to reduce the execution time of the parameter tuning phase. These capabilities are packaged in a Docker container for easy deployment and can be used through a friendly interface extension in 3D Slicer. Our results using three real-world image segmentation workflows demonstrate that the proposed solution is able to (1) search a small fraction (about 100 points) of the parameter space, which contains billions to trillions of points, and improve the quality of segmentation output by × 1.20, × 1.29, and × 1.29, on average; (2) decrease the execution time of a segmentation workflow by up to 11.79× while improving output quality; and (3) effectively use parallel systems to accelerate parameter tuning and segmentation phases. Funding:
|
Ancient Machine Tools for the Construction of the Antikythera Mechanism Parts
|
Publication: Digital Applications in Archaeology and Cultural Heritage. 2019 Jun; 13:e00092. Authors: Aristeidis Voulgaris, Christophoros Mouratidis, Andreas Vossinakis. Institution: Thessaloniki Astronomy Club, Thessaloniki, Greece. Abstract: The present work deals with the study, design, original reconstruction and use of the bow drill of the late archaic period (ca 490 BC), as depicted in two different red figure vases and the vertical lathe depicted on an engraved wall painting of the Petosiris tomb of the Ptolemaic era (300 BC). After the reconstruction of the three ancient tools, during the implementation of the FRAMe Project, their use was thoroughly studied, from which useful conclusions were drawn about the material processing in antiquity, as well as the details of the construction of the Antikythera Mechanism components. Following the new findings detected from the authors’ study of the X-Ray Computed Tomographies from Antikythera Mechanism Research Project, these ancient machine tools can be considered as the progenitors of the Hellenistic period machine tools, which were used for the construction of the mechanical components of the Mechanism. |
Real-Time Adaptive Planning Method for Radiotherapy Treatment Delivery for Prostate Cancer Patients, Based on a Library of Plans Accounting for Possible Anatomy Configuration Changes
|
Publication: PLoS One. 2019 Feb 28;14(2):e0213002. PMID: 30818345 | PDF Authors: Antico M, Prinsen P, Cellini F, Fracassi A, Isola AA, Cobben D, Fontanarosa D. Institution: School of Chemistry, Physics and Mechanical Engineering, Queensland University of Technology, Brisbane, Queensland, Australia. Abstract: BACKGROUND AND PURPOSE: In prostate cancer treatment with external beam radiation therapy (EBRT), prostate motion and internal changes in tissue distribution can lead to a decrease in plan quality. In most currently used planning methods, the uncertainties due to prostate motion are compensated by irradiating a larger treatment volume. However, this could cause underdosage of the treatment volume and overdosage of the organs at risk (OARs). To reduce this problem, in this proof of principle study we developed and evaluated a novel adaptive planning method. The strategy proposed corrects the dose delivered by each beam according to the actual position of the target in order to produce a final dose distribution dosimetrically as similar as possible to the prescribed one. MATERIAL AND METHODS: Our adaptive planning method was tested on a phantom case and on a clinical case. For the first, a pilot study was performed on an in-silico pelvic phantom. A "library" of intensity modulated RT (IMRT) plans corresponding to possible positions of the prostate during a treatment fraction was generated at planning stage. Then a 3D random walk model was used to simulate possible displacements of the prostate during the treatment fraction. At treatment stage, at the end of each beam, based on the current position of the target, the beam from the library of plans, which could reproduce the best approximation of the prescribed dose distribution, was selected and delivered. In the clinical case, the same approach was used on two prostate cancer patients: for the first a tissue deformation was simulated in-silico and for the second a cone beam CT (CBCT) taken during the treatment was used to simulate an intra-fraction change. Then, dosimetric comparisons with the standard treatment plan and, for the second patient, also with an isocenter shift correction, were performed. "...The CT was then elastically deformed on the CBCT using the B-spline method in 3D Slicer." RESULTS: For the phantom case, the plan generated using the adaptive planning method was able to meet all the dosimetric requirements and to correct for a misdosage of 13% of the dose prescription on the prostate. For the first clinical case, the standard planning method caused underdosage of the seminal vesicles, respectively by 5% and 4% of the prescribed dose, when the position changes for the target were correctly taken into account. The proposed adaptive planning method corrected any possible missed target coverage, reducing at the same time the dose on the OARs. For the second clinical case, both with the standard planning strategy and with the isocenter shift correction target coverage was significantly worsened (in particular uniformity) and some organs exceeded some toxicity objectives. While with our approach, the most uniform coverage for the target was produced and systematically the lowest toxicity values for the organs at risk were achieved. CONCLUSIONS: In our proof of principle study, the adaptive planning method performed better than the standard planning and the isocenter shift methods for prostate EBRT. It improved the coverage of the treatment volumes and lowered the dose to the OARs. This planning method is particularly promising for hypofractionated IMRT treatments in which a higher precision and control on dose deposition are needed. Further studies will be performed to test more extensively the proposed adaptive planning method and to evaluate it at a full clinical level. |
Unique Metasomal Musculature in Sweat Bees (Hymenoptera, Apoidea, Halictidae) Revealed by Micro-CT Scanning
|
Publication: American Museum Novitates 2019 Feb; 3920:28 | PDF Authors: Herhold, Hollister W.; Davis, Steven R.; Smith, Corey Shepard.; Engel, Michael S.; Grimaldi, David A. Institution: American Museum of Natural History, New York, NY Abstract: Bees of the family Halictidae (Apoidea: Anthophila) have three pairs of thick, bundled muscles that are circular to subcircular in cross section within the first metasomal segment, as revealed by micro-CT scanning of 16 species in 15 genera of five bee families. In nonhalictids and the basal halictid subfamily Rophitinae, these muscles are planar (flat and sheetlike), typically lying between the anterior air sacs and abdominal wall. In Nomiinae and Halictinae, these muscles, especially the dorsal-ventral pair, bulge into air-sac space, partly enveloped by air-sac membrane. A possible function may be to facilitate metasomal compression and contraction, and thus air flow. The bundled shape of these derived halictid muscles is similar to that of flight muscles, but further data is needed to determine if they are fibrillar, which would suggest a completely different function. "Segmentation and volume rendering was done using 3D Slicer v4.9." |
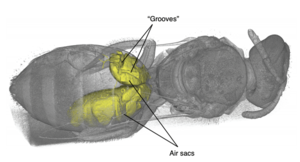 Volume rendering of Lasioglossum (Dialictus) sp. (Halictinae: Halictini), showing location of abdominal air sacs, displayed as a yellow solid, and “grooves” where metasomal muscles extend into the air-sac space. The insect’s exoskeleton and internal anatomy is rendered translucent, allowing examination of air-sac morphology. The bilateral asymmetry shown here is not uncommon, and usually has to do with how recently the specimen has fed. Distension of the gut can occupy space normally taken up by air sacs. |
3D Reconstruction of MR-Visible Fe3O4-Mesh Implants: Pelvic Mesh Measurement Techniques and Preliminary Findings
|
Publication: Neurourol Urodyn. 2019 Jan;38(1):369-78. PMID: 30387537 Authors: Brocker KA, Mokry T, Alt CD, Kauczor HU, Lenz F, Sohn C, DeLancey JO, Chen L. Institution: Department of Obstetrics and Gynecology, Medical School, University of Heidelberg, Heidelberg, Germany. Abstract: AIMS: To develop MR-based measurement technique to evaluate the postoperative dimension and location of implanted magnetic resonance (MR)-visible meshes. METHODS: This technique development study reports findings of six patients (A-F) with cystoceles treated with anterior vaginal MR-visible Fe3O4 -polypropylene implants. Implanted meshes were reconstructed from 3 months and/or 1 year postsurgical MR-images using 3D Slicer. Measurements including mesh length, distance to the ischial spines, pudendal, and obturator neurovascular bundles and urethra were obtained using software Rhino® and a custom Matlab® program. The range of implanted mesh length and their placements were reported and compared with mesh design and implantation recommendations. With the anterior/posterior-mesh-segment-ratio mesh shrinkage localization was evaluated. RESULTS: Examinations were possible for patients A-D 3 months and for A, C, E, and F 1 year postsurgical. The mesh was at least 40% shorter in all patients 3 months and/or 1 year postoperatively. A, B showed shrinkage in the anterior segment, D, E in the posterior segment (Patients C, F not applicable due to intraoperative mesh trimming). Patient E presented pain in the area of mesh shrinkage. In Patient C posterior mesh fixations were placed in the iliococcygeal muscle rather than sacrospinous ligaments. Arm placement less than 20 mm from the pudendal neurovascular bundles was seen in all cases. The portion of the urethra having mesh underneath it ranged from 19% to 55%. CONCLUSIONS: MRI-based measurement techniques have been developed to quantify implanted mesh location and dimension. Mesh placement variations possibly correlating with postoperative complications can be illustrated. Funding:
|
A Complete Workflow for Utilizing Monte Carlo Toolkits in Clinical Cases for a Double-Scattering Proton Therapy System
|
Publication: J Appl Clin Med Phys. 2019 Jan;20(1):23-30. PMID: 30426669 | PDF Authors: Muller L, Prusator M, Ahmad S, Chen Y. Institution: Department of Radiation Oncology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Abstract: The methods described in this paper allow end users to utilize Monte Carlo (MC) toolkits for patient-specific dose simulation and perform analysis and plan comparisons for double-scattering proton therapy systems. The authors aim to fill two aspects of this process previously not explicitly published. The first one addresses the modeling of field-specific components in simulation space. Patient-specific compensator and aperture models are exported from treatment planning system and converted to STL format using a combination of software tools including Matlab and Autodesk's Netfabb. They are then loaded into the MC geometry for simulation purpose. The second details a method for easily visualizing and comparing simulated doses with the dose calculated from the treatment planning system. This system is established by utilizing the open source software 3D Slicer. The methodology was demonstrated with a two-field proton treatment plan on the IROC lung phantom. Profiles and two-dimensional (2D) dose planes through the target isocenter were analyzed using our in-house software tools. This present workflow and set of codes can be easily adapted by other groups for their clinical practice. |
Morphological Analysis of Sigmoid Sinus Anatomy: Clinical Applications to Neurotological Surgery
|
Publication: J Otolaryngol Head Neck Surg. 2019 Jan 11;48(1):2. PMID: 30635049 | PDF Authors: Van Osch K, Allen D, Gare B, Hudson TJ, Ladak H, Agrawal SK. Institution: Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada. Abstract: OBJECTIVES: The primary objective of this study was to use high-resolution micro-CT images to create accurate three-dimensional (3D) models of several intratemporal structures, and to compare several surgically important dimensions within the temporal bone. The secondary objective was to create a statistical shape model (SSM) of a dominant and non-dominant sigmoid sinus (SS) to provide a template for automated segmentation algorithms. METHODS: A free image processing software, 3D Slicer, was utilized to create three-dimensional reconstructions of the SS, jugular bulb (JB), facial nerve (FN), and external auditory canal (EAC) from micro-CT scans. The models were used to compare several clinically important dimensions between the dominant and non-dominant SS. Anatomic variability of the SS was also analyzed using SSMs generated using the Statismo software framework. RESULTS: Three-dimensional models from 38 temporal bones were generated and analyzed. Right dominance was observed in 74% of the paired SSs. All distances were significantly shorter on the dominant side (p < 0.05), including: EAC - SS (dominant: 13.7 ± 3.4 mm; non-dominant: 15.3 ± 2.7 mm), FN - SS (dominant: 7.2 ± 1.8 mm; non-dominant: 8.1 ± 2.3 mm), 2nd genu FN - superior tip of JB (dominant: 8.7 ± 2.2 mm; non-dominant: 11.2 ± 2.6 mm), horizontal distance between the superior tip of JB - descending FN (dominant: 9.5 ± 2.3 mm; non-dominant: 13.2 ± 3.5 mm), and horizontal distance between the FN at the stylomastoid foramen - JB (dominant: 5.4 ± 2.2 mm; non-dominant: 7.7 ± 2.1). Analysis of the SSMs indicated that SS morphology is most variable at its junction with the transverse sinus, and least variable at the JB. CONCLUSIONS: This is the first known study to investigate the anatomical variation and relationships of the SS using high resolution scans, 3D models and statistical shape analysis. This analysis seeks to guide neurotological surgical approaches and provide a template for automated segmentation and surgical simulation. "In 3D Slicer, nine fiducials (F1 – F9) were placed on the 3D reconstructions of the SS, JB, EAC, and FN to analyze several surgically relevant relationships between these structures." Funding:
|
] |